
CLICK THE LINK
What is GLAUCOMA?
Glaucoma is a group of related diseases that damage the optic nerve resulting in vision loss and blindness. Glaucoma is a leading cause of blindness and visual impairment in the United States. Glaucoma can affect patients of all ages. Known as the “sneak thief of sight”, many people affected with glaucoma do not experience any symptoms and may not be aware that they have the disease until they have lost a significant amount of vision.
The eye continually produces a watery substance called aqueous fluid, which constitutes most of the eye. Once made the fluid continually exits the eye through a delicate sieve-like meshwork. Your eye shape is created by the perfect pressure balance maintained by this constant cycle. You will experience an increase in pressure when the drainage system in your eye becomes impaired, this is called Glaucoma. Increased eye pressure is the result of this fluid production versus drainage imbalance. Because of this increased pressure, your vision can be damaged. Therefore early detection and treatment are imperative because your eyes can be protected against the serious loss of vision or blindness with the correct treatment. The Doctors at Eye Associates of South Texas are experts in the treatment of glaucoma by both medical, laser and surgical therapies. This is available at all our clinics in South Texas: San Antonio, Seguin, New Braunfels, La Vernia, Castroville, Hondo, Luling, Lockhart, and Gonzales.
Types of Glaucoma
There are several types of glaucoma with two main types: open-angle and angle-closure.
Symptoms of Glaucoma
Many patients do not experience any symptoms during the early stages of glaucoma, including no pain and no vision loss. This makes it difficult for many patients to know if they have the disease. But as glaucoma progresses, patients may experience some of the following symptoms:
- A loss of peripheral or side vision
- Sudden eye pain
- Headache
- Blurred vision
- The appearance of halos around lights
- Tunnel vision
- Nausea
- Vomiting
- Red eyes
Diagnosing Glaucoma
While some patients may experience symptoms from glaucoma as the disease progresses, others do not realize they have the condition until they undergo a routine eye exam. There are several different exams performed to diagnose glaucoma, including:
- Visual field
- Dilated eye examination
- Retinal evaluation
- Gonioscopy
- Visual acuity test
- Tonometry
- Pachymetry
How is Glaucoma Diagnosed?
At Eye Associates of South Texas, one of our board-certified ophthalmologists or optometrists will use a variety of cutting edge diagnostic instruments and their extensive clinical training to determine whether you have glaucoma.
The Spectral Domain OCT (Zeiss, Optovue, Optos, Nidek) can be used to detect glaucoma without dilation. This newly developed technology produces a comprehensive and accurate optic nerve analysis. This makes early detection and immediate action possible. Your doctor will also measure intraocular pressure, test your peripheral vision, check optic nerve damage and check your eye’s drainage angle during your glaucoma assessment. The visual field will be carefully examined by an automated threshold perimeter also called a Visual Field Analyzer (Humphrey, Heidelberg, Welch Allyn). Color Photographs will document the optic nerve. The corneal thickness will be measured with ultrasonic pachymetry (Accutome). 
Other Testing we will use to aid in your diagnosis:
- Dilated eye examination- to examine your optic nerve stereoscopically
- Retinal evaluation
- Gonioscopy-to determine if you have open or closed-angle glaucoma
- Visual acuity test
- Tonometry
If a second opinion is needed Dr. J.T. Kavanagh MD is a fellowship-trained glaucoma specialist with over 20 years experience in the diagnosis, medical and surgical treatment of glaucoma.
Below is a video showing how severe glaucoma is still not being diagnosed early enough to prevent blindness.
Treatment for Glaucoma
Once glaucoma has been diagnosed, treatment should begin as soon as possible to help minimize the risk of permanent vision loss. There is no cure for glaucoma, so treatment focuses on relieving symptoms and preventing further damage from occurring. The best treatment for your individual case depends on the type of glaucoma and severity of the disease and can be discussed with your doctor. Some of the treatment methods for glaucoma are as follows:
Medication
Medication, either as eye drops or oral medication, is used to either reduce fluid production in the front of the eye or to help drain excess fluid. Side effects of the medication may result in redness, stinging, irritation or blurry vision. Patients should advise their doctor about any medications they are taking or any allergies they have to minimize the risk of side effects. While glaucoma often has no symptoms, regular use of the medication is needed to keep the eye pressure under control.
Surgery
Some cases of glaucoma can be treated with medications. For others, laser or traditional surgery is required to lower eye pressure. Common surgeries include:
At the Eye Associates of South Texas, we are dedicated to providing the best treatments available to our glaucoma patients. Therefore, we offer a range of treatment including minimally invasive glaucoma (MIGS) surgeries. We also are experts at medical treatment of glaucoma and the traditional glaucoma surgeries such as trabeculectomies and Aqueous Shunts with scleral reinforcement grafts.
Minimally Invasive Glaucoma Surgery (MIGS) Types
iStent Inject ®
iStent Inject is a small medical implant that effectively lowers the inside of the eye pressure. The iStent ® device is the smallest medical implant known to have been implanted in the human body. Once the iStent Inject® is implanted into the eye, it works to restore the natural ability of your eye to drain fluid, maintain eye pressure at a safe level, and may allow your doctor to reduce or eliminate your glaucoma medication. The iStent Inject® is a stent for micro-bypass. This means a tiny channel is created through which fluid passes, allowing your eye to drain fluid and avoid high intraocular pressure. During cataract surgery, two iStent Inject® are inserted. The procedure is straightforward. Your surgeon will remove your cataracts during the surgery and then implant the device iStent Inject ®. This is done through a small incision on the surface of the eye. Once the device has been implanted, you won’t see or feel it. You’re going to go home the same day and there’s going to be a quick recovery. The Eye Associates of South Texas became the first eye care practice in San Antonio to perform a post-FDA approval iStent Inject® procedure in August 2018. Watch Dr. Kavanagh’s video on IStent inject.
Hydrus Microstent
The Hydrus Microstent is an Ivantis-made intracanalicular scaffold for open-angle glaucoma treatment. By serving as a scaffold for Schlemm’s canal, the Hydrus Microstent increases fluid outflow throug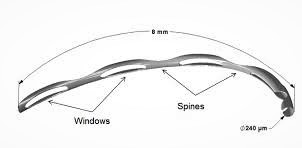 h the trabecular meshwork. The Hydrus Microstent is made of nitinol- a nickel and titanium alloy, it is 8 mm long and highly flexible and biocompatible. The 1 mm inlet segment is located in the anterior chamber and the scaffold segment is located in the channel of Schlemm. Following the surgery, the results of the procedure show a 20% reduction in eye pressure. Like other trabecular meshwork surgeries, there have been hemorrhages that have been resolved in about a week. There has also been some peripheral anterior formation of synechia that has not changed the results. We were the first practice in South Texas and San Antonio to implant the Hydrus micro shunt by Ivantis for glaucoma.
h the trabecular meshwork. The Hydrus Microstent is made of nitinol- a nickel and titanium alloy, it is 8 mm long and highly flexible and biocompatible. The 1 mm inlet segment is located in the anterior chamber and the scaffold segment is located in the channel of Schlemm. Following the surgery, the results of the procedure show a 20% reduction in eye pressure. Like other trabecular meshwork surgeries, there have been hemorrhages that have been resolved in about a week. There has also been some peripheral anterior formation of synechia that has not changed the results. We were the first practice in South Texas and San Antonio to implant the Hydrus micro shunt by Ivantis for glaucoma.
XEN ® Gel Stent
Xen ® Gel Stent is a surgical implant used in patients with open-angle glaucoma to lower intraocular pressure. Usually, this device is used when other treatment methods, such as eye drops or oral medication, have failed. The XEN ® Gel Stent is a small, tube-shaped device that becomes soft and flexible when inserted into the eye. The Xen ® stent works by creating a small fluid drain channel in the eye, from the anterior chamber to the space underneath the skin of the white part of the eye (sclera). Dr. Kavanagh is a certified implanter of the Xen Gel stent, and as a fellowship-trained glaucoma specialist, he finds it a useful tool in his surgical armamentarium against severe glaucoma. Watch his video below.
Dr. Kavanagh has recently started placing the Xen Gel Stent ab Externo, he feels the new approach may improve the surgical outcomes of this procedure.
Kahook Dual Blade Goniotomy 
The Kahook Dual Blade Goniotomy helps surgeons lower intraocular pressure by creating a drainage channel in the eye’s trabecular meshwork (the tissue responsible for draining fluid from the front of the eye). The Kahook Dual Blade Goniotomy helps surgeons lower intraocular pressure. This procedure may be performed during or as a stand-alone procedure during cataract surgery. Your surgeon will use the Kahook dual blade during this procedure to create an incision in the trabecular meshwork, enabling increased drainage of fluids.
Omni Sight Sciences Canaloplasty
Canaloplasty is performed using a second-generation medical device OMNI Surgical System to perform canaloplasty. This decreased resistance to aqueous outflow in the eye lowering intraocular pressure. It can be performed as a stand-alone procedure or in conjunction with cataract surgery. Watch Dr. Kavanagh perform a canaloplasty with the Sight Sciences Device.
Interested in MIGS (Minimally Invasive Glaucoma Surgery)?
If you and your doctor have determined your IOP has not been lowered sufficiently by your glaucoma medication or previous treatments, ask about MIGS! MIGS enables your doctor to treat your glaucoma safely and effectively without any trouble. The difference can be early detection. Call Eye Associates of South Texas to schedule your exam now!
GLAUCOMA LASERS
SLT
Selective Laser Trabeculoplasty (SLT) Selective Laser Trabeculoplasty (SLT) is a clinically proven treatment that can help reduce intraocular pressure (IOP). With short, gentle light bursts, the SLT laser targets pigmented tissue cells within the eye’s drainage system. To cause the least tissue response, the lowest possible laser energy is applied. Because of this, the target tissue has little or no permanent visible change. These laser energy bursts stimulate a natural eye-wide healing response. As a result, the pores through which fluid must exit the eye become larger, resulting in increased fluid outflow, which in turn lowers the pressure of the eye.
In the office, SLT treatments are performed using the same device that the doctor uses to examine patients. Around 80 laser pulses are applied through a special mirrored lens after the eye is numbed with drops. The procedure is not painful, but some patients report a slight pinch, discomfort, or sensation of burning. Any discomfort is mild and usually easily tolerated. While the treatment itself takes only a few minutes, due to preparatory and follow-up measures, the overall process takes about one hour to ensure the eyes of the patient are safe. Only one eye is typically treated at a time. The patient will continue all eye drops and receive a prescription for an eye drop to be used only in the event that after the procedure there is some discomfort. Most patients do not feel that this medication is needed. After laser treatments with SLT, side effects are rare. Below is a list of potential side effects: mild side effects are the most common, including soreness, redness, and vision blurring. Usually, these are very short-lived and can be treated with an eye drop easily and effectively. High eye pressure–In some cases, after the procedure, the eye pressure may increase. Most often, this increase in eye pressure is temporary and can be treated with additional eye drops or oral drugs. This increase in eye pressure can very rarely persist, requiring more invasive surgical procedures. Anterior peripheral synechiae–the iris ‘ adhesion to the cornea. Inflammation & swelling–SLT can cause persistent inflammation within the eye in rare cases. This is a potentially severe complication that may lead to other eye problems.
It should be emphasized that all these side effects of the treatment are very rare. In the unlikely case, they do happen the appropriate treatment will be administered for these complications. Postoperative results vary between individuals for all medical procedures. SLT has the potential to have no effect on the pressure of the eye. The effect can, on the other hand, be marked and last for several years. Depending on the individual circumstances, drops of glaucoma may or may not be needed after the procedure. Continuous monitoring of glaucoma is important, so follow-up appointments are critical. Depending on the results of previous applications, SLT can be replicated safely in the future if necessary.
Watch a video of Lumenis SLT Procedure.
Cyclo G6™ Glaucoma Laser System with MicroPulse P3™ Glaucoma Probe Device
Iridex’s Micropulse P3 is somewhat similar to the original G-Probe cyclodestruction laser except that it provides the ciliary body with a safer treatment method. Instead of a sustained long pulse of laser energy, it is delivered in small bursts. The laser device of MP3 finely controls the application of the laser to the eye. The laser uses micro-pulses of energy to ciliary processes to carry out the transscleral cyclophotocoagulation. This prevents any ocular tissue from heating and burning. Micropulse P3 Cyclophotocoagulation (MP3) is a very successful treatment in some select patients that can reduce the intraocular pressure (IOP) up to 30% in some cases.
Classic Procedures
Trabeculectomy
Involves making a “trap door” into the anterior chamber of the eye, first described by Cairns in the late 1960s. It is a true and tested operation, with a long 50-year track record. Dr. Kavanagh is fellowship trained in glaucoma and routinely performs this surgery when less invasive methods fail to halt glaucoma progression. Watch Dr. Kavanagh’s video of trabeculectomy.
Tube Shunt (Ahmed)
For the worst cases of glaucoma, sometimes an aqueous tube shun is needed.. A device with a tube entering the eye and an external reservoir is required. It is sutured to the sclera. It is usually required in cases of rubeotic or uveitic glaucoma.
The doctors at Eye Associates are also skilled at performing this procedure.
Preventing Glaucoma
There is no way to prevent glaucoma from developing. To prevent glaucoma from progressing, you may want to incorporate some of the following suggestions into your life:
- Get regular comprehensive eye examinations
- Get an annual screening for glaucoma
- Follow the recommended treatment plan from your doctor
- Make healthy lifestyle changes
- Protect your eyes from injury
If you have lost some sight or experience low vision as a result of glaucoma, there are services and programs available that will help you lead a normal, independent life. To learn more about glaucoma and how you can be tested for this serious condition, please call us today to schedule an appointment with one of our skilled eye doctors.

